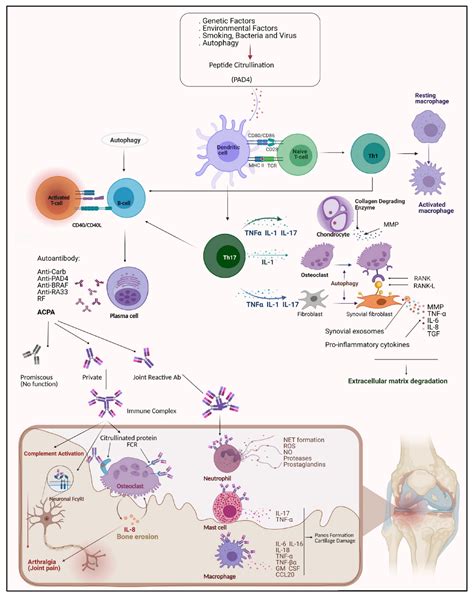
Rheumatoid arthritis (RA) is a complex autoimmune disease characterized by chronic inflammation and joint damage. Its pathogenesis involves a multifaceted interplay of genetic, environmental, immunologic, and other factors. Despite significant advancements in treatment, RA continues to be a major health concern globally.
The pathogenesis of RA involves the UpToDate, as outlined in various studies and articles. These include insights from sources like PubMed, the intersection of genetics and environment as detailed in NCBI Bookshelf, and the comprehensive information provided by the Johns Hopkins Arthritis Center.
Rheumatoid arthritis is not just limited to joint inflammation but also involves systemic symptoms. Early stages of RA typically affect smaller joints, and as the disease progresses, symptoms often spread to larger joints. This progression is detailed in sources like the Mayo Clinic, and the New England Journal of Medicine.
Recent advances in understanding RA’s pathogenesis, including the role of autoantibodies and the autoimmune nature of the disease, have been significant. These developments are captured in publications like MDPI and Nature Immunology.
Significant progress in RA pathogenesis has led to improved treatment options, including the use of targeted biologic and synthetic disease-modifying antirheumatic drugs (DMARDs). However, the disease remains a significant challenge due to its complexity and the varying individual responses to treatments.
Understanding the pathogenesis of rheumatoid arthritis is crucial for developing more effective treatments and improving the quality of life for those affected by this debilitating condition.