The good news is that in most cases — approximately 90% of the time — pain caused by a herniated disc will resolve on its own within six months. Initially, doctors are likely to recommend that patients take over-the-counter pain relievers and limit activities that provoke pain or discomfort.

Microdiscectomy is a surgical option for the relief of pain and other symptoms caused by a herniated disc in the spine pressing on an adjacent nerve root. During this operation, the surgeon removes small fragments of the disc, bone, and ligament, thereby freeing the nerve.
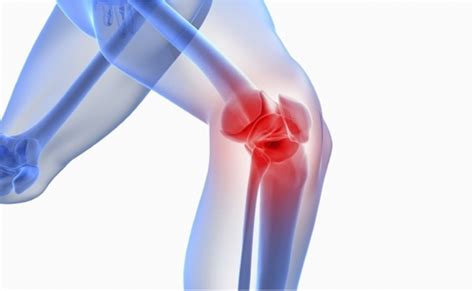
A discectomy, a type of spinal decompression surgery, is another treatment for a herniated disc, which occurs when part of a spinal disc bulges or ruptures, slipping out of place and potentially pressing on a spinal nerve. This condition may lead to neck pain, back and/or leg pain, such as what is experienced in sciatica.
For treating a herniated disc in the lumbar region, several non-surgical options are available before considering surgery, such as weight loss, a tailored physical therapy program, pain medications, and possibly epidural steroid injections.
Most lumbar disc herniations resolve spontaneously without any specific treatment. However, for persistent and painful herniations, treatment typically begins with the least invasive methods, including anti-inflammatory medications and physical therapy.
The initial approach to managing a herniated disc usually involves conservative methods, such as non-steroidal anti-inflammatory drugs (NSAIDs) and rest, which prove sufficient in approximately 80% of cases.
A bulging disc occurs when the outer wall of the disc weakens but does not rupture, leading to an outward bulge. Often, a herniated disc starts as a bulging disc, which then ruptures due to significant pressure. Herniation can happen in the cervical, thoracic, or lumbar spine.
Interestingly, it’s more common to feel pain from a herniated disc in parts of the body other than the back. While a herniated disc in the lower back may sometimes cause pain at the rupture site, it more typically results in pain, weakness, and numbness in the buttocks, legs, or feet due to pressure on the connected nerve.
For more information, visit the following resources: Harvard Health, HSS Microdiscectomy Surgery, HSS Discectomy, HSS Lumbar Disc Herniation FAQs, HSS Herniated Disc, UF Health Lumbar Herniated Disc, and Columbia Neurosurgery Herniated Disc.